Total Knee Replacement - Frequently Asked Questions
Omaha Total Knee Replacement Information by Dr. Ajoy Jana MD
Total Knee Replacement - Frequently Asked Questions
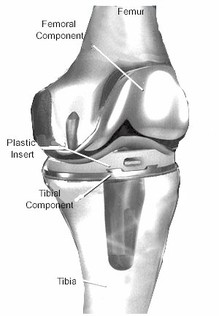
Figure 1. Total Knee Replacement
How do I know if I should have a knee replacement now?
If the pain and stiffness of knee arthritis interferes with your ability to work, enjoy recreational activities, or perform your usual activities of daily living, then knee replacement may be an option for you. Sometimes people make the mistake of believing that they should be nearly incapacitated before having surgery, but the symptoms do not need to be that severe. Of course, knee replacement surgery should not be taken lightly and it’s important to first try the non-surgical treatment options. Your orthopedic surgeon can help you make an informed decision.
Will I do any harm if I put off surgery for a while?
For the vast majority of people, putting off surgery will not harm their knee There are occasional instances, however, when arthritis is severe enough that having surgery sooner rather than later can help prevent further bone or ligament damage. If your knee arthritis is causing a decrease in activity level, then your general health may suffer by delaying surgery.
What exactly is being replaced in a knee replacement?
You can think of your knee like the tire of a car. When the tread on the tire wears out, the tire can be replaced, or it can be re-treaded. Knee replacement is more like re-treading a worn out tire. In a total knee replacement the entire knee joint is not replaced, but rather, the cartilage of the knee is replaced. During the operation, a small amount (about 10mm) of cartilage and bone are removed from the end of the femur (thigh bone), the top of the tibia (shin bone), and the undersurface of the patella (knee cap). The prosthetic parts that are then cemented in place are the same thickness as the bone and cartilage that was removed. A more accurate name for this procedure would have been “total knee resurfacing” or “total knee cartilage replacement.”
How long do knee replacements last?
Lots of factors affect how long a knee replacement will last, but the most important one is your activity level. The more active you are, the faster your knee prosthesis will wear out. Other important factors that can affect the rate of wear include: age, weight, the type of prosthesis and the skill of the surgeon. The Mayo Clinic studied ten thousand patients who had a knee replacement and found that after 20 years, 78% of knee replacements were still functioning while the remaining 22% had needed to be re-done.
If the pain and stiffness of knee arthritis interferes with your ability to work, enjoy recreational activities, or perform your usual activities of daily living, then knee replacement may be an option for you. Sometimes people make the mistake of believing that they should be nearly incapacitated before having surgery, but the symptoms do not need to be that severe. Of course, knee replacement surgery should not be taken lightly and it’s important to first try the non-surgical treatment options. Your orthopedic surgeon can help you make an informed decision.
Will I do any harm if I put off surgery for a while?
For the vast majority of people, putting off surgery will not harm their knee There are occasional instances, however, when arthritis is severe enough that having surgery sooner rather than later can help prevent further bone or ligament damage. If your knee arthritis is causing a decrease in activity level, then your general health may suffer by delaying surgery.
What exactly is being replaced in a knee replacement?
You can think of your knee like the tire of a car. When the tread on the tire wears out, the tire can be replaced, or it can be re-treaded. Knee replacement is more like re-treading a worn out tire. In a total knee replacement the entire knee joint is not replaced, but rather, the cartilage of the knee is replaced. During the operation, a small amount (about 10mm) of cartilage and bone are removed from the end of the femur (thigh bone), the top of the tibia (shin bone), and the undersurface of the patella (knee cap). The prosthetic parts that are then cemented in place are the same thickness as the bone and cartilage that was removed. A more accurate name for this procedure would have been “total knee resurfacing” or “total knee cartilage replacement.”
How long do knee replacements last?
Lots of factors affect how long a knee replacement will last, but the most important one is your activity level. The more active you are, the faster your knee prosthesis will wear out. Other important factors that can affect the rate of wear include: age, weight, the type of prosthesis and the skill of the surgeon. The Mayo Clinic studied ten thousand patients who had a knee replacement and found that after 20 years, 78% of knee replacements were still functioning while the remaining 22% had needed to be re-done.
What is a partial knee replacement and should I have one?
The knee is divided into three compartments (medial, lateral, and patellar). When a person has arthritis in only one of the three compartments of his or her knee, the cartilage of that one compartment can be replaced and this is known as a partial knee replacement. Only about 10% to 15% of patients meet criteria for a partial knee replacement, also known as a unicompartmental or “uni” replacement. The benefit of this operation is that it can be done through a small incision and the recovery is quicker than after a total knee replacement. However, the downside of partial knee replacements is that they usually do not last as long as total knee replacements.
What is a “minimally invasive” total knee replacement?
There are a few surgeons around the country doing total knee replacements through a very small incision (4 inches), but the technique has not yet been perfected nor is it for general use. You will be hard pressed to find an orthopedic surgeon that would choose to have his own knee replaced with this “minimally invasive” technique. Although a partial knee replacement can be done safely through a very small incision, It is much more difficult to do a total knee through one.
If I need both knees replaced, should I have them done at the same time?
Bilateral knee replacements can be done, but this option is reserved only for people in excellent health and with strong motivation to get through the difficult recovery. When both knees are replaced at the same time, the risk of pulmonary embolism, cardiac complications and even death are increased.
What are the possible complications from surgery?
All major surgery has some risk of complications. Most problems that occur are correctable, but some can be quite serious or even life threatening. The following list is not intended to cover all of the possible complications related to knee replacement, but to make you aware of some of the more common ones, as well as the most serious.
Do I need to donate blood for myself prior to surgery?
Self-donation of blood preoperatively is not needed or recommended. Very few patients require a transfusion after knee replacement. Numerous things are done to minimize blood loss and lower the chance of needing a transfusion: a drain is usually used after surgery that captures the patient’s own blood and then this blood is given back as a transfusion six hours after the surgery. We also check to make sure that patients have a good blood count prior to surgery and if they do not a referral is made to the Methodist Hospital Blood Conservation Program. When appropriate, intravenous iron and/or a medicine called Procrit can be used to boost the blood count.
How long does knee replacement surgery take?
The average surgical time is about 75 minutes (usual range is 60-120 minutes). Methodist Hospital provides a nurse liaison to communicate with families and update them during the surgical case, as needed. Lots of factors can affect how long the procedure lasts, including a patient’s size, weight, and severity of arthritis. Keep in mind that the surgery actually starts about 30 minutes from when a patient leaves the pre-operative holding area.
What type of anesthesia will be used?
Knee replacement surgery can be done with either general anesthesia or spinal anesthesia. On the day of surgery, the anesthesiologist can help you decide which choice is best for you. My preference is for spinal anesthesia because it has been shown in studies to have numerous benefits over general anesthesia. The benefits include a lower the risk of blood clots, heart attacks, pneumonia, nausea, and mental impairment. With spinal anesthesia, a shot is given in the lower back to make patients numb below the waist. Sedation is then used so patients sleep through the surgery - this is often referred to as twilight sleep. Most patients who have spinal anesthesia have no memory of their time in the operating room.
Regardless of what type of anesthesia is chosen for the operation, most patients will also receive a femoral and sciatic nerve block prior to surgery to help to lessen the post-operative pain. With these nerve blocks, the anesthesiologist uses a local anesthetic that usually makes the leg feel partially or totally numb for 6-18 hours after surgery. The blocks lessen or even completely eliminate the pain after surgery - until they wear off. Most patients really like the temporary pain relief from the blocks, but many do not like the lack of feeling and strength that comes with the numbing.
Am I going to have a lot of pain after surgery?
There a large differences from person to person with regards to how much pain is experienced. Even though knee replacement is known to be a painful operation, many people are pleasantly surprised at the level of pain they have. Although there is no way to eliminate the pain, by using multi-modal pain management techniques the pain can be minimized.
As noted above, preoperative nerve blocks are used to decrease pain for 6-18 hours after surgery. Medicine is also given pre-operatively and during surgery that has decrease pain and the need for narcotics. After surgery the nurses can give intravenous pain medicine every 2 hours, as needed. Most patients are switched over to oral painkillers after the first night. A combination of long-acting and short-acting pain medicines are often combined with an anti-inflammatory medicine. Most patients take pain medicine for 2-6 weeks after surgery.
How long will I be in the hospital?
Most patients will return home 3 days after surgery. Patients who are recovering slowly or don’t have much help at home may benefit from a short stay in a rehab facility before returning back home. If you need to go to “rehab,” you will be given several options and arrangements will be made by the social worker in the hospital.
What should I look out for when I return home after surgery?
Do not hesitate to call our office or that of your primary care physician if you have any health concerns. These are a few particular things to look out for:
How much Physical Therapy (PT) will I need?
All patients get PT in the hospital twice a day. Upon discharge, we arrange for most patients to have a physical therapist to come to their home 3-5 times per week for the first 2-3 weeks after surgery. After the home therapy, most patients will then be switched over to outpatient Physical Therapy. The total duration of physical therapy is usually 6 to 12 weeks, depending on when all goals are met.
Please remember that the exercises you do independently matter more than the formal Physical Therapy! Your goal in the first 2-3 months after knee replacement is to maximize how far your knee can bend (flexion) and straighten (extension). Our goal is a range-of-motion (ROM) at least as good as your preoperative level and preferably 0-120 degrees. After 3 months, it’s almost impossible to gain significant flexion or extension. So in the beginning, focus on ROM and don’t worry as much about your strength, balance and stamina, as you can work on those later.
How much walking can/should I do when I get home?
The best answer is “as tolerated.” That means gradually increase your activities. Trial and error will tell you how much activity is too much. If you have “overdone it,” then you may experience increased pain and swelling in your leg. Just take it easy for a day or two and then try again at a less intense level. Remember that the healing process takes months, not weeks! Also, keep in mind that your initial goal after knee replacement is to maximize your range-of- motion and it is not to maximize your walking distance.
How long does it take to recover from surgery?
Recovery times vary almost as much as people do. The patients who make the quickest recovery are those in the best general health prior to surgery. Some patients feel better than they did prior to surgery after only a couple of weeks, while others take a three or four months. Most people use a walker or crutches for 2-6 weeks after the operation. By three months after surgery most people are getting along very well. It is normal to have some swelling and mild warmth in the replaced knee for 6 months or more. Improvements in strength, discomfort and swelling can all continue for a full year after surgery.
When can I go back to work?
It depends on what kind of work you do. People with desk jobs and flexible schedules can try to go back to work in a little as a few weeks, though it is usually best to wait for 4-6 weeks. People with jobs that require prolonged standing and full eight-hour days may need to wait for 3 or even 4 months before returning to work.
Will I have to limit my weight bearing?
No. Full weight bearing is permitted right away.
How long do I have to use a walker or crutches?
You can wean yourself off of these supports “as tolerated.” After surgery, your leg muscles will be weak and there will be some pain, so the support is necessary. Usually your Physical Therapist can help advise you when to transition away from the support. Remember that it’s better to walk smoothly with a cane than to limp around without one, as walking with a limp can result in back or hip pain.
Do I have to be careful about the position that I sleep?
No. You should feel free to sleep in any position that you are comfortable. When you are asleep, you have no control over the position of your knee, so I think that it is futile to try to keep the knee straight when you are sleeping. If you have worked hard during the day to exercise your knee, you should be able to rest guilt-free without worrying about your knee position. On a related note, many patients do seem to have some trouble getting a good night sleep after surgery, but this seems to resolve after a few months.
When can I stop wearing my TED hose?
The compression stockings (TED hose) help decrease swelling in the leg and reduce the risk of blood clots. I prefer that patients wear them on the operative leg for 2 weeks following surgery. Feel free to remove them while in bed each night and then replace them in the morning.
When can I stop taking the blood thinner?
In most cases, the blood thinner can be discontinued 2 weeks after surgery. Patients who are at higher risk of blood clots are kept on blood thinners 4-6 weeks. If you were taking a daily aspirin prior to surgery, it can be restarted once you are out of the hospital.
When can I drive again?
There is no fixed amount of time that driving is prohibited. In general, when your driving leg has good strength and control and you are no longer taking pain medicine such as Hydrocodone (Norco), or Oxycodone (Percocet), then it should be okay to drive.
Are there any travel restrictions after surgery?
It is best not to take any long trips for three months after surgery. While not an absolute requirement, this advice is given because the risk of blood clots remains higher than normal for about 3 months after knee replacement, and prolonged sitting in a car or plane can add to this risk.
When can I shower or bathe?
The initial surgical dressing is usually replaced two days after the surgery with a special waterproof dressing. With this new dressing you can shower right away. This dressing is designed to be left in place for one week and then it can be removed. At that point, most patients no longer need any dressing. You should, however, avoid taking baths or swimming until given the okay - usually 3 weeks after surgery. If a standard dressing was used then showers can start once the wound is cry and no longer draining any fluid.
Will I be allowed to kneel down?
Yes, when your incision is completely healed. It will probably take at least 3 months before you will want to try to kneel down. Unfortunately, most people never regain the ability to kneel comfortably directly on the knee. If you must kneel, a good quality kneepad can help a lot.
Will I be able to play sports and exercise again?
Regular exercise is encouraged. However, people with joint replacements should avoid high-impact types of exercise and sports (i.e., jogging or basketball). Golf and doubles tennis can be resumed 3 – 6 months after surgery. The goal of knee replacement is to eliminate or decrease pain so that you can remain active, but too much activity will certainly cause the knee replacement to wear out more quickly. There is no way to say exactly how much activity is too much. I recommend no lifting or carrying more than 50 pounds.
Is it normal for my knee replacement to “click” or “grind”?
Yes, it is completely normal and harmless. Almost everyone notices some “clicking” in his or her artificial knee. The sound comes from the metal and plastic parts of the knee bumping together. Grinding sounds come from scar tissue that often forms after surgery. If the grinding is painful then let you should let us know.
Is it normal for my knee to have a numb spot on the skin?
Everyone who has a knee replacement will have a small area of skin that remains numb permanently. The area is adjacent to the incision, below the kneecap and it occurs because there is a small nerve that must be cut when the surgery is done. Right after surgery, it is also common to have some numbness around the entire incision, but over time most of that numbness will go away.
If I want to have my other knee replaced, how long should I wait in between surgeries?
It is usually best to wait a minimum of three months in between surgeries to give yourself adequate time to recover from the first surgery.
Will I need to return for any follow-up after my recovery is complete?
Yes. X-rays can pick up signs of wear or loosening long before you feel any discomfort and therefore should be checked regularly. The frequency of follow-up will be based on your activity level and it can vary from visits once a year to once every five years.
Will I set off metal detectors at the airport?
Yes, most people with knee replacements do set off the metal detector. Simply tell the TSA agent that you have had a knee replacement. If you set off the metal detector, the agent is required to pull you aside and check you using a “wand.” Unfortunately, there is no TSA-approved identification card that states that you have had a knee replacement.
Is it true I’ll have to take antibiotics before any dental work?
Yes. For a minimum of two years after a total joint replacement it is recommended that you take a single dose of oral antibiotic before any procedure that can introduce bacteria into your blood stream. This includes dental work, colonoscopy, cystoscopy (bladder ‘scope), and some other procedures. This is to prevent “seeding” of your artificial joint by bacteria, resulting in an infection. I prefer that my patients continue this practice indefinitely.
The knee is divided into three compartments (medial, lateral, and patellar). When a person has arthritis in only one of the three compartments of his or her knee, the cartilage of that one compartment can be replaced and this is known as a partial knee replacement. Only about 10% to 15% of patients meet criteria for a partial knee replacement, also known as a unicompartmental or “uni” replacement. The benefit of this operation is that it can be done through a small incision and the recovery is quicker than after a total knee replacement. However, the downside of partial knee replacements is that they usually do not last as long as total knee replacements.
What is a “minimally invasive” total knee replacement?
There are a few surgeons around the country doing total knee replacements through a very small incision (4 inches), but the technique has not yet been perfected nor is it for general use. You will be hard pressed to find an orthopedic surgeon that would choose to have his own knee replaced with this “minimally invasive” technique. Although a partial knee replacement can be done safely through a very small incision, It is much more difficult to do a total knee through one.
If I need both knees replaced, should I have them done at the same time?
Bilateral knee replacements can be done, but this option is reserved only for people in excellent health and with strong motivation to get through the difficult recovery. When both knees are replaced at the same time, the risk of pulmonary embolism, cardiac complications and even death are increased.
What are the possible complications from surgery?
All major surgery has some risk of complications. Most problems that occur are correctable, but some can be quite serious or even life threatening. The following list is not intended to cover all of the possible complications related to knee replacement, but to make you aware of some of the more common ones, as well as the most serious.
- Death is a very rare complication but it should still be mentioned. As with any major surgery, death could occur from such things as heart attack, stroke, pneumonia or anesthesia.
- Infection: The chance of getting a deep infection around the prosthesis following total knee replacement is approximately 1%. Although the risk is small, infection following joint replacement surgery can be a particularly serious complication - often requiring intensive antibiotic treatment and additional surgery. Some infections may show up very early, before even leaving the hospital, while others may not become apparent for months, or even years after an operation. It is important to know that infection can spread to an artificial knee from any part of the body that has infection. That’s why it is so important to make sure any infection in your body is treated urgently. That is also why it is recommended that people who have an artificial joint take a prophylactic antibiotic before having dental work or any surgical procedure with a risk of bacterial contamination.
- Blood clots (deep vein thromboses or DVT) can form in the large veins of the leg after knee replacement. This may cause the leg to swell, become warm to the touch and painful. A blood clot in the lungs is called a pulmonary embolism (PE) and it can come from a clot that starts in the legs or it can form in the lungs directly. A PE can be very serious and even cause death. One of the most effective ways to reduce the risk of DVT and PE is to get out of bed and start moving soon after surgery. In addition, patients are placed on a blood thinner for 2-4 weeks after surgery.
- Injuries to nerves or blood vessels are very rare, but can occur because these structures are near the knee joint. The most common type of nerve injury results in temporary or permanent inability to pull the foot upward (a “foot drop”).
- Persistent stiffness or loss of range of motion can occur. While most people equal or improve upon their pre-surgery range of motion, some patients don’t. Normal healing after any surgery involves scar tissue formation. Unfortunately, some patients form too much scar tissue and that causes the knee to become very stiff. It is essential to vigorously exercise the knee after surgery in order to restore range of motion. Unfortunately a few percent of patients are unable to regain good movement despite working hard at rehabilitation.
- There are some patients who have persistent pain despite an otherwise successful surgery. When this occurs it is very frustrating and disappointing for both the patient and the surgeon.
- Post-operative confusion and memory loss can result from narcotic pain medicines and anesthesia especially in older patients. Understandably, families are often caught off-guard when this happens and it can be quite upsetting to witness. When it occurs, it usually lasts two or three days.
Do I need to donate blood for myself prior to surgery?
Self-donation of blood preoperatively is not needed or recommended. Very few patients require a transfusion after knee replacement. Numerous things are done to minimize blood loss and lower the chance of needing a transfusion: a drain is usually used after surgery that captures the patient’s own blood and then this blood is given back as a transfusion six hours after the surgery. We also check to make sure that patients have a good blood count prior to surgery and if they do not a referral is made to the Methodist Hospital Blood Conservation Program. When appropriate, intravenous iron and/or a medicine called Procrit can be used to boost the blood count.
How long does knee replacement surgery take?
The average surgical time is about 75 minutes (usual range is 60-120 minutes). Methodist Hospital provides a nurse liaison to communicate with families and update them during the surgical case, as needed. Lots of factors can affect how long the procedure lasts, including a patient’s size, weight, and severity of arthritis. Keep in mind that the surgery actually starts about 30 minutes from when a patient leaves the pre-operative holding area.
What type of anesthesia will be used?
Knee replacement surgery can be done with either general anesthesia or spinal anesthesia. On the day of surgery, the anesthesiologist can help you decide which choice is best for you. My preference is for spinal anesthesia because it has been shown in studies to have numerous benefits over general anesthesia. The benefits include a lower the risk of blood clots, heart attacks, pneumonia, nausea, and mental impairment. With spinal anesthesia, a shot is given in the lower back to make patients numb below the waist. Sedation is then used so patients sleep through the surgery - this is often referred to as twilight sleep. Most patients who have spinal anesthesia have no memory of their time in the operating room.
Regardless of what type of anesthesia is chosen for the operation, most patients will also receive a femoral and sciatic nerve block prior to surgery to help to lessen the post-operative pain. With these nerve blocks, the anesthesiologist uses a local anesthetic that usually makes the leg feel partially or totally numb for 6-18 hours after surgery. The blocks lessen or even completely eliminate the pain after surgery - until they wear off. Most patients really like the temporary pain relief from the blocks, but many do not like the lack of feeling and strength that comes with the numbing.
Am I going to have a lot of pain after surgery?
There a large differences from person to person with regards to how much pain is experienced. Even though knee replacement is known to be a painful operation, many people are pleasantly surprised at the level of pain they have. Although there is no way to eliminate the pain, by using multi-modal pain management techniques the pain can be minimized.
As noted above, preoperative nerve blocks are used to decrease pain for 6-18 hours after surgery. Medicine is also given pre-operatively and during surgery that has decrease pain and the need for narcotics. After surgery the nurses can give intravenous pain medicine every 2 hours, as needed. Most patients are switched over to oral painkillers after the first night. A combination of long-acting and short-acting pain medicines are often combined with an anti-inflammatory medicine. Most patients take pain medicine for 2-6 weeks after surgery.
How long will I be in the hospital?
Most patients will return home 3 days after surgery. Patients who are recovering slowly or don’t have much help at home may benefit from a short stay in a rehab facility before returning back home. If you need to go to “rehab,” you will be given several options and arrangements will be made by the social worker in the hospital.
What should I look out for when I return home after surgery?
Do not hesitate to call our office or that of your primary care physician if you have any health concerns. These are a few particular things to look out for:
- Signs of Infection: You or a family member should check the incision every day for signs of infection. While it is normal for the area around the incision and staples to be a little pink and even a little warm, it should not be red or hot. If there is ever redness that seems to be spreading you need to contact our office immediately or go to the Methodist Hospital Emergency Department. Fever and/or increasing pain in the knee can also be signs of infection and need prompt medical evaluation.
- Blood clot (DVT) in a leg vein can cause the leg to swell and become more painful. Everyone’s leg has some swelling after surgery, but if the amount of swelling suddenly increases and especially if the swelling doesn’t improve after elevating the leg, then you should call our office or go to the Emergency Department. A pulmonary embolism can cause chest pain, shortness of breath, and rapid heart rate and requires immediate attention.
- Constipation: Pain medicines (narcotics) can cause constipation. It helps to eat a high fiber diet and consider taking an over-the-counter stool softener Colace daily. If needed, consider also using a laxative such as Milk of Magnesia or Dulcolax and contact your primary care physician for further treatment as needed.
How much Physical Therapy (PT) will I need?
All patients get PT in the hospital twice a day. Upon discharge, we arrange for most patients to have a physical therapist to come to their home 3-5 times per week for the first 2-3 weeks after surgery. After the home therapy, most patients will then be switched over to outpatient Physical Therapy. The total duration of physical therapy is usually 6 to 12 weeks, depending on when all goals are met.
Please remember that the exercises you do independently matter more than the formal Physical Therapy! Your goal in the first 2-3 months after knee replacement is to maximize how far your knee can bend (flexion) and straighten (extension). Our goal is a range-of-motion (ROM) at least as good as your preoperative level and preferably 0-120 degrees. After 3 months, it’s almost impossible to gain significant flexion or extension. So in the beginning, focus on ROM and don’t worry as much about your strength, balance and stamina, as you can work on those later.
How much walking can/should I do when I get home?
The best answer is “as tolerated.” That means gradually increase your activities. Trial and error will tell you how much activity is too much. If you have “overdone it,” then you may experience increased pain and swelling in your leg. Just take it easy for a day or two and then try again at a less intense level. Remember that the healing process takes months, not weeks! Also, keep in mind that your initial goal after knee replacement is to maximize your range-of- motion and it is not to maximize your walking distance.
How long does it take to recover from surgery?
Recovery times vary almost as much as people do. The patients who make the quickest recovery are those in the best general health prior to surgery. Some patients feel better than they did prior to surgery after only a couple of weeks, while others take a three or four months. Most people use a walker or crutches for 2-6 weeks after the operation. By three months after surgery most people are getting along very well. It is normal to have some swelling and mild warmth in the replaced knee for 6 months or more. Improvements in strength, discomfort and swelling can all continue for a full year after surgery.
When can I go back to work?
It depends on what kind of work you do. People with desk jobs and flexible schedules can try to go back to work in a little as a few weeks, though it is usually best to wait for 4-6 weeks. People with jobs that require prolonged standing and full eight-hour days may need to wait for 3 or even 4 months before returning to work.
Will I have to limit my weight bearing?
No. Full weight bearing is permitted right away.
How long do I have to use a walker or crutches?
You can wean yourself off of these supports “as tolerated.” After surgery, your leg muscles will be weak and there will be some pain, so the support is necessary. Usually your Physical Therapist can help advise you when to transition away from the support. Remember that it’s better to walk smoothly with a cane than to limp around without one, as walking with a limp can result in back or hip pain.
Do I have to be careful about the position that I sleep?
No. You should feel free to sleep in any position that you are comfortable. When you are asleep, you have no control over the position of your knee, so I think that it is futile to try to keep the knee straight when you are sleeping. If you have worked hard during the day to exercise your knee, you should be able to rest guilt-free without worrying about your knee position. On a related note, many patients do seem to have some trouble getting a good night sleep after surgery, but this seems to resolve after a few months.
When can I stop wearing my TED hose?
The compression stockings (TED hose) help decrease swelling in the leg and reduce the risk of blood clots. I prefer that patients wear them on the operative leg for 2 weeks following surgery. Feel free to remove them while in bed each night and then replace them in the morning.
When can I stop taking the blood thinner?
In most cases, the blood thinner can be discontinued 2 weeks after surgery. Patients who are at higher risk of blood clots are kept on blood thinners 4-6 weeks. If you were taking a daily aspirin prior to surgery, it can be restarted once you are out of the hospital.
When can I drive again?
There is no fixed amount of time that driving is prohibited. In general, when your driving leg has good strength and control and you are no longer taking pain medicine such as Hydrocodone (Norco), or Oxycodone (Percocet), then it should be okay to drive.
Are there any travel restrictions after surgery?
It is best not to take any long trips for three months after surgery. While not an absolute requirement, this advice is given because the risk of blood clots remains higher than normal for about 3 months after knee replacement, and prolonged sitting in a car or plane can add to this risk.
When can I shower or bathe?
The initial surgical dressing is usually replaced two days after the surgery with a special waterproof dressing. With this new dressing you can shower right away. This dressing is designed to be left in place for one week and then it can be removed. At that point, most patients no longer need any dressing. You should, however, avoid taking baths or swimming until given the okay - usually 3 weeks after surgery. If a standard dressing was used then showers can start once the wound is cry and no longer draining any fluid.
Will I be allowed to kneel down?
Yes, when your incision is completely healed. It will probably take at least 3 months before you will want to try to kneel down. Unfortunately, most people never regain the ability to kneel comfortably directly on the knee. If you must kneel, a good quality kneepad can help a lot.
Will I be able to play sports and exercise again?
Regular exercise is encouraged. However, people with joint replacements should avoid high-impact types of exercise and sports (i.e., jogging or basketball). Golf and doubles tennis can be resumed 3 – 6 months after surgery. The goal of knee replacement is to eliminate or decrease pain so that you can remain active, but too much activity will certainly cause the knee replacement to wear out more quickly. There is no way to say exactly how much activity is too much. I recommend no lifting or carrying more than 50 pounds.
Is it normal for my knee replacement to “click” or “grind”?
Yes, it is completely normal and harmless. Almost everyone notices some “clicking” in his or her artificial knee. The sound comes from the metal and plastic parts of the knee bumping together. Grinding sounds come from scar tissue that often forms after surgery. If the grinding is painful then let you should let us know.
Is it normal for my knee to have a numb spot on the skin?
Everyone who has a knee replacement will have a small area of skin that remains numb permanently. The area is adjacent to the incision, below the kneecap and it occurs because there is a small nerve that must be cut when the surgery is done. Right after surgery, it is also common to have some numbness around the entire incision, but over time most of that numbness will go away.
If I want to have my other knee replaced, how long should I wait in between surgeries?
It is usually best to wait a minimum of three months in between surgeries to give yourself adequate time to recover from the first surgery.
Will I need to return for any follow-up after my recovery is complete?
Yes. X-rays can pick up signs of wear or loosening long before you feel any discomfort and therefore should be checked regularly. The frequency of follow-up will be based on your activity level and it can vary from visits once a year to once every five years.
Will I set off metal detectors at the airport?
Yes, most people with knee replacements do set off the metal detector. Simply tell the TSA agent that you have had a knee replacement. If you set off the metal detector, the agent is required to pull you aside and check you using a “wand.” Unfortunately, there is no TSA-approved identification card that states that you have had a knee replacement.
Is it true I’ll have to take antibiotics before any dental work?
Yes. For a minimum of two years after a total joint replacement it is recommended that you take a single dose of oral antibiotic before any procedure that can introduce bacteria into your blood stream. This includes dental work, colonoscopy, cystoscopy (bladder ‘scope), and some other procedures. This is to prevent “seeding” of your artificial joint by bacteria, resulting in an infection. I prefer that my patients continue this practice indefinitely.
Connect with me on Google +