Total Knee Replacement - Frequently Asked Questions
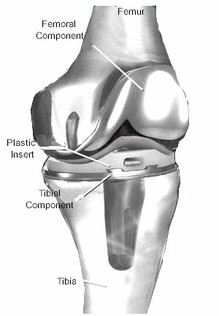
Figure 1. Total Knee Replacement
What is arthritis and how did I get it?
Joint cartilage is the smooth, slippery, rubber-like covering at the ends of a bone. Arthritis simply refers to the thinning and eventual loss of joint cartilage. Typical symptoms include pain, swelling, stiffness, “catching,” and limp.
How will I know when it's time to have a knee replacement?
When severe arthritis affects your quality of life – by interfering with your ability to work, to enjoy recreational activities or to perform your activities of daily living - then you may be a candidate for a knee replacement. Of course, it’s important to make a full attempt at medical treatment of your arthritis before turning to surgical treatment. Through shared decision making, your orthopedic surgeon can help advise you when surgery is a reasonable option, but the final decision on whether to have surgery is yours to make.
Will I do any harm if I put off surgery for a while?
For most patients, delaying surgery will not harm the knee joint or make future surgery any harder. For those rare cases where a patient’s arthritis is extreme and bone damage is occurring, surgery may be recommended right away.
But if my knee hurts, why wouldn't I want to have a knee replacement now?
Basically, there are three reasons not to rush into a knee replacement: 1) they don’t last forever 2) not everyone who has a knee replacement is happy with it and 3) complications can occur with any surgery.
What exactly is being replaced in a total knee replacement?
Many patients have a misunderstanding of what is done during a total knee replacement. It is the worn-out cartilage of the knee joint that is replaced, not the entire knee. A more accurate name for this procedure would have been “total knee cartilage replacement.” During the operation, 8-10 mm of cartilage and bone are removed from each of the 3 bones of the knee - the end of the femur, the top of the tibia, and the back of the patella. The prosthetic replacement parts are then cemented in place. See diagram:
Joint cartilage is the smooth, slippery, rubber-like covering at the ends of a bone. Arthritis simply refers to the thinning and eventual loss of joint cartilage. Typical symptoms include pain, swelling, stiffness, “catching,” and limp.
- Osteoarthritis (OA), also known as degenerative arthritis, is the most common type of arthritis. The factors that influence who gets this disease include age, genetics, physical labor and body weight. For some patients, the cause is unknown.
- Rheumatoid arthritis (RA) is an auto-immune disease that causes severe inflammation of the lining (synovium) of the joint and this causes destruction of the joint cartilage.
- Post-traumatic arthritis can develop after fractures, dislocations and ligament injuries.
How will I know when it's time to have a knee replacement?
When severe arthritis affects your quality of life – by interfering with your ability to work, to enjoy recreational activities or to perform your activities of daily living - then you may be a candidate for a knee replacement. Of course, it’s important to make a full attempt at medical treatment of your arthritis before turning to surgical treatment. Through shared decision making, your orthopedic surgeon can help advise you when surgery is a reasonable option, but the final decision on whether to have surgery is yours to make.
Will I do any harm if I put off surgery for a while?
For most patients, delaying surgery will not harm the knee joint or make future surgery any harder. For those rare cases where a patient’s arthritis is extreme and bone damage is occurring, surgery may be recommended right away.
But if my knee hurts, why wouldn't I want to have a knee replacement now?
Basically, there are three reasons not to rush into a knee replacement: 1) they don’t last forever 2) not everyone who has a knee replacement is happy with it and 3) complications can occur with any surgery.
What exactly is being replaced in a total knee replacement?
Many patients have a misunderstanding of what is done during a total knee replacement. It is the worn-out cartilage of the knee joint that is replaced, not the entire knee. A more accurate name for this procedure would have been “total knee cartilage replacement.” During the operation, 8-10 mm of cartilage and bone are removed from each of the 3 bones of the knee - the end of the femur, the top of the tibia, and the back of the patella. The prosthetic replacement parts are then cemented in place. See diagram:
What are knee replacements made of?
The metal parts are made of an alloy containing mostly cobalt, chromium and nickel (usually just called “cobalt-chrome”). Titanium is not used much for knee replacements because it is too soft and scratches easily. There is always a polyethylene (plastic) part that is used on the tibia and patella in place of the cartilage. Allergies to these metals are very rare, but if you think you may be allergic to any type of metal, please let your surgeon know.
How successful are knee replacements nowadays?
It is very important to have realistic expectations about knee replacement. Studies on patient-reported outcomes show that about 90% of patients who have knee replacement are satisfied, while about 10% of patients are dissatisfied. Even satisfied patients do not necessarily have a knee that feels completely normal - about half still have some residual symptoms such as mild stiffness, discomfort, or swelling. Patients should expect some clicking or grinding noises with knee movement and intermittent swelling with activity is also common. Most patients will not be able to kneel comfortably and all patients have some numbness on the front of the knee. Nevertheless, knee replacement remains the best option when other treatments have failed.
What is a partial knee replacement and should I have one?
The knee is divided into three compartments. When a person has arthritis in only one of the three compartments, a partial knee replacement may be an option. Only about 10% of patients could even consider this option. Although the recovery is a little quicker for a partial knee replacement, total knee replacements generally last many years longer.
How long do knee replacements last?
Your age, activity level and body weight are the biggest factors determining how long a knee replacement will last. The Mayo Clinic studied ten thousand patients who had a knee replacement and found that after 20 years, 78% of knee replacements were still functioning but the remaining 22% had worn out. The data on the right is from the United Kingdom and it shows how knee replacements in younger patients wear out faster than in older patients.
What happens if my knee replacement does wear out eventually?
Knee replacements typically wear out in one of two ways – either the plastic (polyethylene) on the tibia wears down (like the tread on your car tires) or the bond between the bone, cement, and implant loosens. Either way, a loose or worn out prosthesis can be revised to a new one, but this second surgery is usually more complex and has more risks.
If I need both knees replaced, should I have them done at the same time?
For most patients, it is better to replace one knee at a time. The second knee can be replaced as soon as three months later, after allowing enough time for recovery from the first one. To be a candidate for bilateral (double) knee replacement, you should be in excellent health and have the right frame-of-mind to get through the more difficult recovery. The benefits of bilateral knee replacement include less total time doing rehab and less total time off from work. However, the benefits have to be weighed against the higher risk of medical complications.
What type of anesthesia will be used?
Knee replacement surgery can be done with either general anesthesia or spinal anesthesia. When possible, spinal anesthesia is preferred because it is associated with a lower risk of blood clots, heart attacks, pneumonia, nausea and mental impairment. Some patients are unsure about getting spinal anesthesia because they think it involves being awake during surgery, when in fact patients are heavily sedated (twilight sleep) once the spinal block is given, and most have no memory of their time in the operating room. On the day of surgery, your anesthesiologist will discuss both options with you and then you can decide.
What are the risks associated with knee replacement surgery?
All major surgeries come with some risk of complications. Most problems that occur are correctable, but some can be quite serious or even life threatening. The following list is not intended to cover all the possible complications related to knee replacement, but to make you aware of the more common ones, as well as the most serious.
We use something called “multi-modal” pain management techniques to minimize post-operative pain as much as possible. Of course, everyone’s pain tolerance is different, but by using multiple different medications that prevent and treat pain, most patients achieve very good pain control. On average, patients take an opioid pain medicine for 2 - 8 weeks after surgery. A good rule-of-thumb is that you should take the minimum amount of pain medicine needed to adequately control your pain. Our practice policy is that we will not prescribe any opioid pain medicines after 3 months.
How long does surgery take?
Most patients are in the operating room for about 1 1/2 hours, with the actual surgical time averaging about 60 minutes. Some cases take longer depending on a patient’s size and severity of arthritis. During the surgery, a nurse liaison is available in the waiting area to communicate with families and update them as needed.
How long will I be in the hospital?
Most patients return home 1 to 3 days after surgery, with most going home after 2 nights. Patients who are recovering slowly or don’t have help at home may benefit from a short stay in a Skilled Nursing Facility (SNF). If you need to go to a SNF for further rehabilitation, the hospital social worker will help make the arrangements.
When can I shower or bathe?
Studies show that showering does not increase the risk of infection, so patients can shower even before going home from the hospital. Most patients go home with a waterproof dressing that should be removed after one week. Even after the dressing is removed it is okay to shower. Patients can get in a tub or pool 4 weeks after surgery as long as the incision is completely healed.
How much Physical Therapy (PT) will I need?
Most patients will work with a Physical Therapist for 6 weeks after surgery, but the total duration will depend on when goals are met. When discharged to home, either home or outpatient PT will be prescribed.
What should I look out for when I return home after surgery?
Do not hesitate to call our office or that of your primary care physician if you have any health concerns. These are a few things to look out for:
How much walking can/should I do when I get home?
In the first two weeks, it is best to walk 10-15 minutes every hour. As the healing continues, gradually increase your activities. Trial and error will tell you how much activity is too much. Expect to have some good days and some bad days and remember that the healing process takes months, not weeks! Also, keep in mind that your immediate goal after knee replacement is to maximize your range-of-motion rather than your walking distance.
When can I stop wearing my compression (TED) hose?
The compression stockings (TED hose) help decrease swelling in the leg and reduce the risk of blood clots. I prefer that patients wear them for 2 weeks following surgery. The TED hose can and should be removed periodically during the day when your legs are elevated, as well as each night before going to bed.
Do ice-packs help?
Most patients find that cold-therapy is a good pain reliever. Freezable gel packs are a good option because they are both convenient and help prevent over-freezing of the skin. Please remember that the use of cold-therapy is optional and you should therefore not feel obligated to use it if you don’t like the cold. If you do find it useful, be sure to limit use to 30 minutes at a time, off and on throughout the day, and keep a layer of protection over the skin to avoid frost-bite.
How long do I have to use a walker?
You are permitted to wean off the walker as soon as you feel ready. For most patients, it is best to transition to a cane before walking without any support. Some patients can start weaning themselves off the walker after just a few days, while others take a few weeks. Remember that it’s better to walk smoothly with a cane than to limp around without one - walking with a limp can cause pain in your back or other joints.
When can I go back to work?
It depends on what kind of work you do. People with sedentary jobs and flexible schedules can try to go back to work in 4-6 weeks. People with jobs that require prolonged standing and full eight-hour days may need to wait for 3 or even 4 months before returning to work.
When can I drive again?
Most patients should not drive the first 2 weeks after surgery. After that, my rule-of-thumb is that patients can resume driving when they have good leg strength and have stopped taking opioid pain medicine such as Hydrocodone (Norco) or Oxycodone (Percocet).
How long does it take to recover from surgery?
Complete recovery takes a full year, but most people are back to normal daily activities after 3 months. Every patient heals at a different rate, but being physically fit helps speed up the process. The graph at right shows the typical rate that healing occurs after surgery. Surprisingly, younger patients often take longer than older patients to feel fully recovered. It is normal to have some swelling and mild warmth in the replaced knee for 6 months or more.
When can I stop taking blood thinner?
Specific instruction will be given at the time of discharge from the hospital. When aspirin is used, it can be discontinued 4 weeks after surgery. Numerous recent studies have shown that aspirin prevents symptomatic blood clots as effectively as stronger blood thinners with less expense and less risk of major bleeding. For higher-risk patients who are put on a stronger blood thinner, the duration is usually 6 weeks. An acid-blocking medicine is usually prescribed to help protect your stomach while on blood thinners.
Will I be able to play sports and exercise again?
After knee replacement, regular exercise is encouraged. However, patients should avoid heavy lifting and high-impact exercise and sports. That means no more jogging or basketball and no lifting more than 50 lbs. Golf and doubles tennis can be resumed 3 months after surgery. Keep in mind that even though exercise is good, there is no way to say exactly how much activity is too much - moderation is the key. Like the tires on your car, your knee replacement will wear out proportional to how much wear and tear you put on it.
Will I be able to kneel?
You will be allowed to kneel, but most patients never find kneeling comfortable after knee replacement. Wait at least 3 months before trying. A good quality knee-pad or piece of foam can help a lot.
Will I need to return for any follow-up after my recovery is complete?
Yes, x-rays can pick up signs of wear or loosening before you feel any discomfort and therefore should be checked periodically. The frequency of follow-up will be based on your activity level.
Are there any travel restrictions after surgery?
It is best not to take any long trips for 2-3 months after surgery. Short trips of 1-2 hours duration should be okay after 6 weeks. This advice is given because the risk of blood clots remains higher than normal for about 3 months after knee replacement, and prolonged sitting in a car or plane can add to this risk.
Will I set off metal detectors at the airport?
Yes, most people with knee replacements do set off the metal detector. Simply tell the TSA agent that you have had a knee replacement. If you set off the metal detector, the TSA agent is required to pull you aside for additional screening. It does not help to have an identification card that states that you have had a knee replacement, as anyone could easily make a counterfeit card.
Will I have to take antibiotics before any dental work?
Yes, the current recommendation is that for two years after surgery healthy patients should take an antibiotic before any procedure that can introduce bacteria into the blood stream such as dental work and colonoscopy. Patients who are considered high-risk will be asked to continue this practice of prophylactic antibiotics indefinitely. Either your dentist’s office or our office can provide the prescription.
What should I do to get ready for surgery?
To minimize your risks and maximize your recovery you can do the following: exercise as much as possible, lose weight if you are overweight, stop smoking if you are a smoker, complete any necessary dental work and if you are currently taking an opioid pain medicine, try to wean off before surgery. These things can make a very big difference in your recovery.
Disclaimer: The above information is for patient education only and reflects the views of the author. Every person is different and so every patient’s experience with surgery will be different. You and your physician should develop a plan of care that is unique to your individual needs.
The metal parts are made of an alloy containing mostly cobalt, chromium and nickel (usually just called “cobalt-chrome”). Titanium is not used much for knee replacements because it is too soft and scratches easily. There is always a polyethylene (plastic) part that is used on the tibia and patella in place of the cartilage. Allergies to these metals are very rare, but if you think you may be allergic to any type of metal, please let your surgeon know.
How successful are knee replacements nowadays?
It is very important to have realistic expectations about knee replacement. Studies on patient-reported outcomes show that about 90% of patients who have knee replacement are satisfied, while about 10% of patients are dissatisfied. Even satisfied patients do not necessarily have a knee that feels completely normal - about half still have some residual symptoms such as mild stiffness, discomfort, or swelling. Patients should expect some clicking or grinding noises with knee movement and intermittent swelling with activity is also common. Most patients will not be able to kneel comfortably and all patients have some numbness on the front of the knee. Nevertheless, knee replacement remains the best option when other treatments have failed.
What is a partial knee replacement and should I have one?
The knee is divided into three compartments. When a person has arthritis in only one of the three compartments, a partial knee replacement may be an option. Only about 10% of patients could even consider this option. Although the recovery is a little quicker for a partial knee replacement, total knee replacements generally last many years longer.
How long do knee replacements last?
Your age, activity level and body weight are the biggest factors determining how long a knee replacement will last. The Mayo Clinic studied ten thousand patients who had a knee replacement and found that after 20 years, 78% of knee replacements were still functioning but the remaining 22% had worn out. The data on the right is from the United Kingdom and it shows how knee replacements in younger patients wear out faster than in older patients.
What happens if my knee replacement does wear out eventually?
Knee replacements typically wear out in one of two ways – either the plastic (polyethylene) on the tibia wears down (like the tread on your car tires) or the bond between the bone, cement, and implant loosens. Either way, a loose or worn out prosthesis can be revised to a new one, but this second surgery is usually more complex and has more risks.
If I need both knees replaced, should I have them done at the same time?
For most patients, it is better to replace one knee at a time. The second knee can be replaced as soon as three months later, after allowing enough time for recovery from the first one. To be a candidate for bilateral (double) knee replacement, you should be in excellent health and have the right frame-of-mind to get through the more difficult recovery. The benefits of bilateral knee replacement include less total time doing rehab and less total time off from work. However, the benefits have to be weighed against the higher risk of medical complications.
What type of anesthesia will be used?
Knee replacement surgery can be done with either general anesthesia or spinal anesthesia. When possible, spinal anesthesia is preferred because it is associated with a lower risk of blood clots, heart attacks, pneumonia, nausea and mental impairment. Some patients are unsure about getting spinal anesthesia because they think it involves being awake during surgery, when in fact patients are heavily sedated (twilight sleep) once the spinal block is given, and most have no memory of their time in the operating room. On the day of surgery, your anesthesiologist will discuss both options with you and then you can decide.
What are the risks associated with knee replacement surgery?
All major surgeries come with some risk of complications. Most problems that occur are correctable, but some can be quite serious or even life threatening. The following list is not intended to cover all the possible complications related to knee replacement, but to make you aware of the more common ones, as well as the most serious.
- The most frequent “complication” of a knee replacement is simply not being happy with the final result. About 5-10% of patients who have a knee replacement feel that it was not a success – usually because of continued pain or stiffness. Unfortunately, a bad outcome can happen despite both the surgeon and the patient doing everything “right.”
- Infection. The chance of getting an infection following a total knee replacement is approximately ½% to 1%. Although the risk is small, infection following joint replacement surgery can be a particularly serious complication - often requiring intensive antibiotic treatment and additional surgery. While some knee infections may show up before leaving the hospital, others may not become apparent for weeks, months or even years after an operation. Because infection can spread into the replaced knee from an infection anywhere in the body, seek immediate treatment if you suspect that you have an infection.
- Stiffness. Most patients after knee replacement have a final range-of-motion (ROM) that is the same or better than before surgery. For some reason, probably genetic, a small percentage of patients heal with excessive scar tissue that causes the knee to become stiffer than before surgery. It is essential to vigorously exercise the knee after surgery, but doing so does not completely guarantee good ROM.
- Injuries to nerves or blood vessels are very rare, but can occur because these structures are near the knee joint. Everyone with a knee replacement has an area of numbness on the front of the knee.
- Delayed wound healing can occur in patients with poor circulation due to vascular disease or smoking. Also, diabetes, obesity and rheumatoid arthritis increase the chances of slow wound healing.
- Blood transfusion is rarely needed nowadays and it would only be given when the benefits are felt to outweigh the potential risks.
- Post-operative confusion and memory loss can result from opioid pain medicines and anesthesia. When it does occur, patients and families are often caught off-guard and find the experience quite upsetting. Most of the time the symptoms resolve in 2 or 3 days.
- Constipation or ileus (temporary bowel shut-down) can also result from opioid pain medicines and anesthesia. To lower the risk, we recommend the routine use of laxatives after surgery and careful monitoring of bowel habits.
- Mechanical complications of the implant rarely occur. However, if you live long enough, everyone should expect that the knee prosthesis will eventually wear out and need to be revised.
- Cardiac issues can arise from the strain of surgery and anesthesia, but mostly in patients who have a pre-existing condition. Examples include atrial fibrillation, congestive heart failure or heart attack (MI).
- Death is a very rare complication. As with any major surgery, death could occur from such things as heart attack, stroke, pulmonary embolism or anesthesia.
We use something called “multi-modal” pain management techniques to minimize post-operative pain as much as possible. Of course, everyone’s pain tolerance is different, but by using multiple different medications that prevent and treat pain, most patients achieve very good pain control. On average, patients take an opioid pain medicine for 2 - 8 weeks after surgery. A good rule-of-thumb is that you should take the minimum amount of pain medicine needed to adequately control your pain. Our practice policy is that we will not prescribe any opioid pain medicines after 3 months.
How long does surgery take?
Most patients are in the operating room for about 1 1/2 hours, with the actual surgical time averaging about 60 minutes. Some cases take longer depending on a patient’s size and severity of arthritis. During the surgery, a nurse liaison is available in the waiting area to communicate with families and update them as needed.
How long will I be in the hospital?
Most patients return home 1 to 3 days after surgery, with most going home after 2 nights. Patients who are recovering slowly or don’t have help at home may benefit from a short stay in a Skilled Nursing Facility (SNF). If you need to go to a SNF for further rehabilitation, the hospital social worker will help make the arrangements.
When can I shower or bathe?
Studies show that showering does not increase the risk of infection, so patients can shower even before going home from the hospital. Most patients go home with a waterproof dressing that should be removed after one week. Even after the dressing is removed it is okay to shower. Patients can get in a tub or pool 4 weeks after surgery as long as the incision is completely healed.
How much Physical Therapy (PT) will I need?
Most patients will work with a Physical Therapist for 6 weeks after surgery, but the total duration will depend on when goals are met. When discharged to home, either home or outpatient PT will be prescribed.
What should I look out for when I return home after surgery?
Do not hesitate to call our office or that of your primary care physician if you have any health concerns. These are a few things to look out for:
- Infection. You or a family member should check your incision every day for signs of infection. Post-surgical bruising, inflammation and swelling can make the knee feel warm and look discolored or pink. But if there is ever redness that is spreading, a fever above 100.5 F, drainage of puss, or progressively increasing pain, contact our office immediately. There is always a surgeon available to advise you.
- Blood clots. Everyone can expect to have some degree of knee and leg swelling after surgery, but we ask patients to call our office if they experience a large or sudden increase in leg swelling or pain – especially if it does not improve with elevation of the leg. To rule out a deep vein thrombosis (DVT), we may need to order an ultrasound. A pulmonary embolism (PE) is a blood clot in the lungs that can cause chest pain, shortness of breath, and/or rapid heart rate and requires immediate attention in a hospital.
- Constipation. Opioid pain medicines usually cause constipation. While it helps to eat a high fiber diet and drink enough fluid, most patients should also take a mild laxative daily – MiraLAX and/or Senokot-S are good options. If needed, consider adding Milk of Magnesia or Dulcolax or even an enema. Contact your primary care physician for further treatment as needed.
How much walking can/should I do when I get home?
In the first two weeks, it is best to walk 10-15 minutes every hour. As the healing continues, gradually increase your activities. Trial and error will tell you how much activity is too much. Expect to have some good days and some bad days and remember that the healing process takes months, not weeks! Also, keep in mind that your immediate goal after knee replacement is to maximize your range-of-motion rather than your walking distance.
When can I stop wearing my compression (TED) hose?
The compression stockings (TED hose) help decrease swelling in the leg and reduce the risk of blood clots. I prefer that patients wear them for 2 weeks following surgery. The TED hose can and should be removed periodically during the day when your legs are elevated, as well as each night before going to bed.
Do ice-packs help?
Most patients find that cold-therapy is a good pain reliever. Freezable gel packs are a good option because they are both convenient and help prevent over-freezing of the skin. Please remember that the use of cold-therapy is optional and you should therefore not feel obligated to use it if you don’t like the cold. If you do find it useful, be sure to limit use to 30 minutes at a time, off and on throughout the day, and keep a layer of protection over the skin to avoid frost-bite.
How long do I have to use a walker?
You are permitted to wean off the walker as soon as you feel ready. For most patients, it is best to transition to a cane before walking without any support. Some patients can start weaning themselves off the walker after just a few days, while others take a few weeks. Remember that it’s better to walk smoothly with a cane than to limp around without one - walking with a limp can cause pain in your back or other joints.
When can I go back to work?
It depends on what kind of work you do. People with sedentary jobs and flexible schedules can try to go back to work in 4-6 weeks. People with jobs that require prolonged standing and full eight-hour days may need to wait for 3 or even 4 months before returning to work.
When can I drive again?
Most patients should not drive the first 2 weeks after surgery. After that, my rule-of-thumb is that patients can resume driving when they have good leg strength and have stopped taking opioid pain medicine such as Hydrocodone (Norco) or Oxycodone (Percocet).
How long does it take to recover from surgery?
Complete recovery takes a full year, but most people are back to normal daily activities after 3 months. Every patient heals at a different rate, but being physically fit helps speed up the process. The graph at right shows the typical rate that healing occurs after surgery. Surprisingly, younger patients often take longer than older patients to feel fully recovered. It is normal to have some swelling and mild warmth in the replaced knee for 6 months or more.
When can I stop taking blood thinner?
Specific instruction will be given at the time of discharge from the hospital. When aspirin is used, it can be discontinued 4 weeks after surgery. Numerous recent studies have shown that aspirin prevents symptomatic blood clots as effectively as stronger blood thinners with less expense and less risk of major bleeding. For higher-risk patients who are put on a stronger blood thinner, the duration is usually 6 weeks. An acid-blocking medicine is usually prescribed to help protect your stomach while on blood thinners.
Will I be able to play sports and exercise again?
After knee replacement, regular exercise is encouraged. However, patients should avoid heavy lifting and high-impact exercise and sports. That means no more jogging or basketball and no lifting more than 50 lbs. Golf and doubles tennis can be resumed 3 months after surgery. Keep in mind that even though exercise is good, there is no way to say exactly how much activity is too much - moderation is the key. Like the tires on your car, your knee replacement will wear out proportional to how much wear and tear you put on it.
Will I be able to kneel?
You will be allowed to kneel, but most patients never find kneeling comfortable after knee replacement. Wait at least 3 months before trying. A good quality knee-pad or piece of foam can help a lot.
Will I need to return for any follow-up after my recovery is complete?
Yes, x-rays can pick up signs of wear or loosening before you feel any discomfort and therefore should be checked periodically. The frequency of follow-up will be based on your activity level.
Are there any travel restrictions after surgery?
It is best not to take any long trips for 2-3 months after surgery. Short trips of 1-2 hours duration should be okay after 6 weeks. This advice is given because the risk of blood clots remains higher than normal for about 3 months after knee replacement, and prolonged sitting in a car or plane can add to this risk.
Will I set off metal detectors at the airport?
Yes, most people with knee replacements do set off the metal detector. Simply tell the TSA agent that you have had a knee replacement. If you set off the metal detector, the TSA agent is required to pull you aside for additional screening. It does not help to have an identification card that states that you have had a knee replacement, as anyone could easily make a counterfeit card.
Will I have to take antibiotics before any dental work?
Yes, the current recommendation is that for two years after surgery healthy patients should take an antibiotic before any procedure that can introduce bacteria into the blood stream such as dental work and colonoscopy. Patients who are considered high-risk will be asked to continue this practice of prophylactic antibiotics indefinitely. Either your dentist’s office or our office can provide the prescription.
What should I do to get ready for surgery?
To minimize your risks and maximize your recovery you can do the following: exercise as much as possible, lose weight if you are overweight, stop smoking if you are a smoker, complete any necessary dental work and if you are currently taking an opioid pain medicine, try to wean off before surgery. These things can make a very big difference in your recovery.
Disclaimer: The above information is for patient education only and reflects the views of the author. Every person is different and so every patient’s experience with surgery will be different. You and your physician should develop a plan of care that is unique to your individual needs.