What is arthritis and how did I get it?
Joint cartilage is the smooth, slippery, rubber-like covering at the ends of a bone. Hip arthritis simply refers to the thinning and eventual loss of joint cartilage. Typical symptoms include pain, stiffness, “catching,” and limp.
How do I know when I should have a hip replacement?
When severe arthritis affects your quality of life – by interfering with your ability to work, to enjoy recreational activities or to perform your activities of daily living - then you may be a candidate for a hip replacement. Of course, it’s important to make a full attempt at medical treatment of your arthritis before turning to surgical treatment. Through shared decision making, your orthopedic surgeon can help advise you when surgery is a reasonable option, but the final decision on whether to have surgery is yours to make.
What exactly is being replaced in a hip replacement?
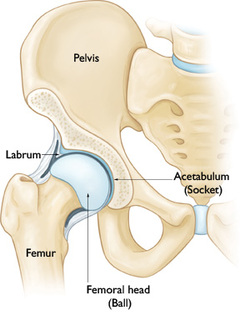
The hip joint is a ball-and-socket joint. During a hip replacement, the head of the femur is removed and replaced with a prosthetic ball which is attached to a stem that is inserted into the femur. The acetabulum is replaced with a metal and plastic (polyethylene) socket. See diagram:
Joint cartilage is the smooth, slippery, rubber-like covering at the ends of a bone. Hip arthritis simply refers to the thinning and eventual loss of joint cartilage. Typical symptoms include pain, stiffness, “catching,” and limp.
- Osteoarthritis (OA), also known as degenerative arthritis, is the most common type of arthritis. The factors that influence who gets this disease include age, genetics, physical labor and body weight. For some patients, the cause is unknown.
- Rheumatoid arthritis (RA) is a type of auto-immune disease that causes severe inflammation of the lining (synovium) of the joint and this causes progressive destruction of the joint cartilage.
- Post-traumatic arthritis can develop after fractures, dislocations and severe contusions.
- Avascular necrosis (AVN), also known as osteonecrosis, occurs when insufficient blood flow to the head of the femur causes areas of the bone to die and collapse. The most common causes of AVN are heavy alcohol use, high-dose steroids, severe trauma or simply no reason at all.
- Dysplasia refers to a shallow socket or abnormally shaped femoral head that is present from birth.
- Perthes Disease (a type of childhood AVN) and Slipped Capital Femoral Epiphysis (a slipped growth plate) are hip problems that occur during childhood or adolescence.
How do I know when I should have a hip replacement?
When severe arthritis affects your quality of life – by interfering with your ability to work, to enjoy recreational activities or to perform your activities of daily living - then you may be a candidate for a hip replacement. Of course, it’s important to make a full attempt at medical treatment of your arthritis before turning to surgical treatment. Through shared decision making, your orthopedic surgeon can help advise you when surgery is a reasonable option, but the final decision on whether to have surgery is yours to make.
What exactly is being replaced in a hip replacement?
The hip joint is a ball-and-socket joint. During a hip replacement, the head of the femur is removed and replaced with a prosthetic ball which is attached to a stem that is inserted into the femur. The acetabulum is replaced with a metal and plastic (polyethylene) socket. See diagram:
Total Hip Replacement - Frequently Asked Questions
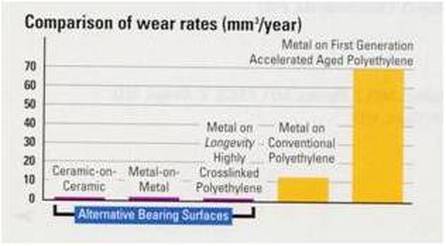
Figure 3. Comparison of wear rates
What are hip replacements made of?
The femoral stem and acetabular shell are made of a titanium alloy. Titanium is a very “bone friendly” metal and when it is implanted tightly in the bone, the bone will fuse right to it. The acetabular liner is a highly-crosslinked polyethylene (plastic) that is very durable. The femoral head is either made from metal (cobalt-chrome-nickel) or ceramic. Almost no one has an allergy to titanium or ceramic, but if you think you may be allergic to any type of metal, please let your surgeon know.
So how successful are hip replacements nowadays?
The good news is that hip replacements have a very high rate of patient satisfaction. That being said, it is still important to have realistic expectations. Studies on patient-reported outcomes show that about 95% of patients who have hip replacement are satisfied, while about 5% of patients are dissatisfied. Even the patients who are satisfied with the surgery do not necessarily have a hip that feels completely normal - some patients have residual symptoms such as mild stiffness, discomfort, or limp. Most patients do return to normal activities and low-impact exercise.
Will I do any harm if I put off surgery for a while?
For most patients, delaying surgery will not harm the hip joint or make future surgery any harder. For those rare cases where a patient’s arthritis is extreme and bone damage is occurring, surgery may be recommended right away. In general, younger patients should try to put off hip replacement for as long as they reasonably can because hip replacements don’t last forever.
How long do hip replacements last?
Activity level and body weight are the most important factors affecting how long the hip prosthesis will last. The more active you are, the faster it will wear out, so moderation is key. Because of technological advances, we are hopeful that most hip replacements will last 20-30 years, and possibly longer.
What happens if my hip replacement does wear out eventually?
It is expected that the plastic acetabular liner will wear out eventually (20+ years) and when that happens the old liner and femoral head can be replaced - while leaving the rest of the original prosthesis in place. The femoral stem and acetabular shell can also loosen from the bone, but luckily that happens less often. Any loose part of the prosthesis can and will need to be replaced. The most common symptom of a loose or worn out implant is pain. Revision surgeries are usually more complex and do have a higher risk of complications.
Can I have the “minimally invasive” hip replacement?
I use the direct anterior surgical approach for almost all my hip replacements. Some people refer to this as “minimally invasive” hip replacement, but I do not like that description. All hip replacements are major operations, so I don’t want my patients to think otherwise. That being said, the direct anterior approach allows me to do hip replacement surgery without cutting any muscle. Studies have shown that this can result in:
• Faster return to a normal gait
• Lower risk of dislocation - no need for the traditional 6 weeks of restrictions.
• More accurate prosthesis placement - intra-operative x-rays help ensure equal leg lengths and proper prosthesis alignment and fit.
• Smaller incision – usually just 5” long
• Less pain
What if I can’t have the direct anterior surgical approach?
For the small fraction of patients who are not good candidates for the direct anterior approach, I usually use the posterior approach. This is the most commonly used surgical approach in the US and it has worked well for decades. This approach is best when the hip surgery is complicated by such factors as morbid obesity, extreme stiffness or revision surgery. When fully healed, the final result should be the same.
How long does surgery take?
Most patients are in the operating room for about 2 hours, with the actual surgical time averaging about 75 minutes. Some cases take longer depending on a patient’s size and severity of arthritis. During the surgery, a nurse liaison is available in the waiting area to communicate with families and update them as needed.
If I need both hips replaced, should I have them done at the same time?
I do not recommend bilateral hip replacements due to the increased risk involved. I feel it is best to wait a minimum of 3 months between surgeries to give adequate time for recovery from the first operation.
What type of anesthesia is used?
Hip replacement surgery can be done with either general anesthesia or spinal anesthesia. When possible, spinal anesthesia is preferred because it is associated with a lower risk of blood clots, heart attacks, pneumonia, nausea and mental impairment. Some patients are unsure about getting spinal anesthesia because they think it involves being awake during surgery, when in fact patients are heavily sedated (twilight sleep) once the spinal block is given, and most have no memory of their time in the operating room. On the day of surgery, your anesthesiologist will discuss both options with you and then you can decide.
What are the risks associated with hip replacement surgery?
All major surgeries come with some risk of complications. Most problems that occur are correctable, but some can be quite serious or even life threatening. The following list is not intended to cover all the possible complications related to hip replacement, but to make you aware of the more common ones, as well as the most serious.
• Infection. The chance of getting an infection following a total hip replacement is approximately ½%. Although the risk is small, infection following joint replacement surgery can be a particularly serious complication - often requiring intensive antibiotic treatment and additional surgery. While some hip infections may show up before leaving the hospital, others may not become apparent for weeks, months or even years after the operation. Because infection can spread into the replaced hip from an infection anywhere in the body, it’s important to seek immediate treatment if you suspect you have any infection.
• Hip dislocation occurs when the femoral head (hip ball) comes out of the hip socket. This used to be the most common complication of hip replacement, but with the direct anterior approach the risk has been reduced to less than ½ %. When the posterior approach is used, there is still a 2-4% risk of dislocation and with revision hip replacements, the dislocation risk can be as high as 15%.
• Leg length difference. Every attempt is made to equalize leg length during surgery, but it is sometimes necessary to lengthen the leg that is being operated on in order to prevent future dislocation. Certain patients have an unstable hip that could dislocate unless the leg is made a little longer. This is more likely to happen in women than men due to women’s more loose ligaments and muscles. By my estimate, a noticeable post-surgical difference in leg length only happens in about 1% of men and 5% of women. The difference is typically less than 5mm if it occurs at all.
• Delayed wound healing can occur due to pressure on the skin by the surgical retractors. This does occur more frequently with the direct anterior approach because the surgery is done through a tighter surgical “window.” It is more likely to happen in patients who are obese, diabetic or smokers.
• Fracture of the femur or pelvis can occur during or occasionally after surgery. In most cases, the fracture can be recognized and fixed immediately without affecting the final result.
• Mechanical complications. The titanium prosthesis needs to fuse to the bone and this happens reliably in almost every patient. In the rare instance that this fusion does not occur successfully, another surgery would be required. The hip prosthesis is very durable and almost never breaks, but after years (decades) of wear-and-tear it is expected to eventually wear out.
• Post-operative confusion and memory loss can result from opioid pain medicines and anesthesia. When it does occur, patients and families are often caught off-guard and find the experience quite upsetting. Most of the time the symptoms resolve in 2 or 3 days.
• Constipation or ileus (temporary bowel shut-down) can also result from opioid pain medicines and anesthesia. Routine use of laxatives and careful monitoring of bowel habits after surgery can help to lower the risk.
• Injuries to nerves or blood vessels are very rare, but can occur during surgery because these structures are located near the hip joint. The risk of some degree of thigh numbness is higher for the direct anterior approach than other surgical approaches because the incision is closer to branches of the femoral nerve. Most patients do experience some numbness around the incision area, but it typically decreases over time. Nerve damage effecting muscle strength is very uncommon and usually temporary.
• Limp. A mild limp may persist, even after fully recovering from hip replacement surgery.
• Persistent pain is unusual, but can happen at times. Even though the joint has been replaced, pain in the hip area can be a consequence of low back arthritis, spinal stenosis or muscle dysfunction. About 75% patients end up with a completely pain-free hip, but it’s important to understand that it is still considered normal and expected to have some mild aches or discomfort after hip replacement. Studies have shown that up to 10% of patients have some activity-related thigh pain.
• Blood transfusion is rarely needed nowadays and it would only be given when the benefits are felt to outweigh the potential risks.
• Cardiac issues can arise from the strain of surgery and anesthesia, but mostly in patients who have a pre-existing condition. Examples include atrial fibrillation, congestive heart failure or heart attack (MI).
• Death is a very rare complication. As with any major surgery, death can occur from such things as heart attack, stroke, pulmonary embolism or anesthesia.
How much pain should I expect after surgery?
We use something called “multi-modal” pain management techniques to minimize post-operative pain as much as possible. Of course, everyone’s pain tolerance is different, but by using the muscle-sparing anterior surgical approach and combining it with multiple different medications that prevent and treat pain, most patients achieve very good pain control. On average, patients take an opioid pain medicine for 1 - 6 weeks after surgery. A good rule-of-thumb is that you should take the minimum amount of pain medicine needed to adequately control your pain. Our practice policy is that we will not prescribe any opioid pain medicines after 3 months.
How long will I be in the hospital?
Most patients return home 1 to 2 days after surgery. Patients who are recovering slowly or don’t have help at home may benefit from a short stay in a Skilled Nursing Facility (SNF). If you need to go to a SNF for further rehabilitation, the hospital social worker will help make the arrangements.
Do ice-packs help?
Most patients find that cold-therapy is a good pain reliever. Freezable gel packs are a good option because they are both convenient and help prevent over-freezing of the skin. Please remember that the use of cold-therapy is optional and you should therefore not feel obligated to use it if you don’t like the cold. If you do find it useful, be sure to limit use to 30 minutes at a time, off and on throughout the day, and keep a layer of protection over the skin to avoid frost-bite.
How much physical therapy (PT) will I have?
Physical therapy will be individualized based on a patient’s needs. For patients who discharge directly to home, I’ve found that most do very well exercising independently for the first 4-6 weeks, without the need for formal PT. After 4-6 weeks, I generally recommend a short course of outpatient PT. Of course, those patients who need home PT or a short stay in a rehab center will have those arrangements made for them in the hospital.
How long do I have to use a walker?
You are permitted to wean off the walker as soon as you feel ready. For most patients, it is best to transition to a cane before walking without any support. Some patients can start weaning themselves off the walker after just a few days, while others take a few weeks. Remember that it’s better to walk smoothly with a cane than to limp around without one - walking with a limp can cause pain in your back or other joints.
How much walking can/should I do when I get home?
For the first 2 weeks after surgery it is good to stand or walk for 10-20 minutes every hour, but not much more than that. Between 2 weeks and 6 weeks after surgery limit your walking to 30 minutes. After 6 weeks, you can advance your activity as tolerated without limitations - trial and error will tell you how much activity is too much. If you overdo it, then you may experience increased pain and swelling in your leg, but rest will usually resolve the setback in a day or two. Remember that complete healing takes months, not weeks.
How long does it take to fully recover from surgery?
Complete recovery takes a full year, but most people are back to normal daily activities after 3 months. Every patient heals at a different rate, but being physically fit helps speed up the process. The graph at right shows the typical rate that healing occurs after surgery. Surprisingly, younger patients often take longer than older patients to feel fully recovered.
What should I look out for when I return home after surgery?
Do not hesitate to call our office or your primary care physician if you have any health concerns after surgery. These are a few things to look out for:
• Infection. You or a family member should check your incision every day for signs of infection. Post-surgical bruising, inflammation and swelling can make the hip feel warm and look discolored or pink. But if there is ever redness that is spreading, a fever above 100.5 F, drainage of puss, or progressively increasing pain, contact our office immediately. There is always a surgeon available to advise you.
• Blood clots. Everyone can expect to have some degree of hip and leg swelling after surgery, but we ask patients to call our office if they experience a large or sudden increase in leg swelling or pain – especially if it does not improve with elevation of the leg. To rule out a deep vein thrombosis (DVT), we may need to order an ultrasound. A pulmonary embolism (PE) is a blood clot in the lungs that can cause chest pain, shortness of breath, and/or rapid heart rate and requires immediate attention in a hospital.
• Constipation. Opioid pain medicines usually cause constipation. While it helps to eat a high fiber diet and drink enough fluid, most patients should also take a mild laxative daily – MiraLAX and/or Senokot-S are good options. If needed, consider adding Milk of Magnesia or Dulcolax or even an enema. Contact your primary care physician for further treatment as needed.
Do I have to restrict my hip movement after surgery?
If you’ve had anterior approach hip replacement, you will NOT have any restrictions on your hip movement. You can bend over, cross your legs and sit in any comfortable chair you like. You can sleep on your side and resume sexual activity whenever you are comfortable. Most patients who have had the posterior approach will be asked to follow hip dislocation precautions. If dislocation precautions are needed, the physical therapists at Methodist Hospital will teach them to you prior to discharge.
When can I stop taking the blood thinner?
Specific instruction will be given at the time of discharge from the hospital. When aspirin is used, it can be discontinued 4 weeks after surgery. Numerous recent studies have shown that aspirin prevents symptomatic blood clots as effectively as stronger blood thinners with less expense and less risk of major bleeding. For higher-risk patients who are put on a stronger blood thinner, the duration is usually 6 weeks. An acid-blocking medicine is usually prescribed to help protect your stomach while on blood thinners.
When can I stop wearing my compression stockings (TED hose)?
Compression stockings (TED hose) help decrease swelling in the leg and reduce the risk of blood clots. I prefer that patients wear them for 2 weeks following surgery. The TED hose can and should be removed periodically during the day when your legs are elevated, as well as each night before going to bed.
When can I shower or bathe?
Studies show that showering does not increase the risk of infection, so patients can shower even before going home from the hospital. Most patients go home with a waterproof dressing that should be removed after one week. Even after the dressing is removed it is okay to shower. Patients can get in a tub or pool 4 weeks after surgery as long as the incision is completely healed.
When can I drive again?
Most patients should not drive the first 2 weeks after surgery. After that, my rule-of-thumb is that patients can resume driving when they have good leg strength and have stopped taking opioid pain medicine such as Hydrocodone (Norco) or Oxycodone (Percocet).
When can I go back to work?
It depends on what kind of work you do. People with sedentary jobs and flexible schedules can try to go back to work in a few weeks. People with jobs that require prolonged standing and full eight-hour days may need to wait 3 or even 4 months before returning to work.
Will I be able to play sports and exercise again?
After hip replacement, regular exercise is encouraged. However, patients should avoid heavy lifting and high-impact exercise and sports. That means no more jogging or basketball and no lifting more than 50 lbs. Golf and doubles tennis can be resumed 3 months after surgery. Keep in mind that even though exercise is good, there is no way to say exactly how much activity is too much - moderation is the key. Like the tires on your car, your hip replacement will wear out proportional to how much wear-and-tear you put on it.
Are there any travel restrictions after surgery?
It is best not to take any long trips for 2-3 months after surgery. Short trips of 1-2 hours duration should be okay after 6 weeks. This advice is given because the risk of blood clots remains higher than normal for about 3 months after hip replacement, and prolonged sitting in a car or plane can add to this risk.
Will I set off metal detectors at the airport?
Yes, most people with hip replacements do set off the metal detector. Simply tell the TSA agent that you have had a hip replacement. If you set off the metal detector, be aware that the TSA agent is required to pull you aside for additional screening. It does not help to have an identification card that states that you have had a hip replacement, as anyone could easily make a counterfeit card.
Will I need to return for any follow-up after my recovery is complete?
Yes. X-rays should be checked periodically because they can pick up signs of wear or loosening of the hip prosthesis before you would feel any discomfort. Frequency of follow-up will be based on your activity level.
Will I have to take antibiotics before dental work?
Yes, the current recommendation is that for two years after surgery healthy patients should take an antibiotic before any procedure that can introduce bacteria into the blood stream such as dental work and colonoscopy. Patients who are considered high-risk will be asked to continue this practice of prophylactic antibiotics indefinitely. Either your dentist’s office or our office can provide the prescription.
What should I do to get ready for surgery?
To minimize your risks and maximize your recovery you can do the following:
• exercise as much as possible
• lose weight if you are overweight
• stop smoking if you are a smoker
• complete any necessary dental work
• if you are currently taking an opioid pain medicine, try to wean off before surgery.
Disclaimer: The above information is for patient education only and reflects the views of the author. Every person is different and so every patient’s experience with surgery will be different. You and your physician should develop a plan of care that is unique to your individual needs.